Advanced Wound Care Solutions
Multiple Allografts to Choose From
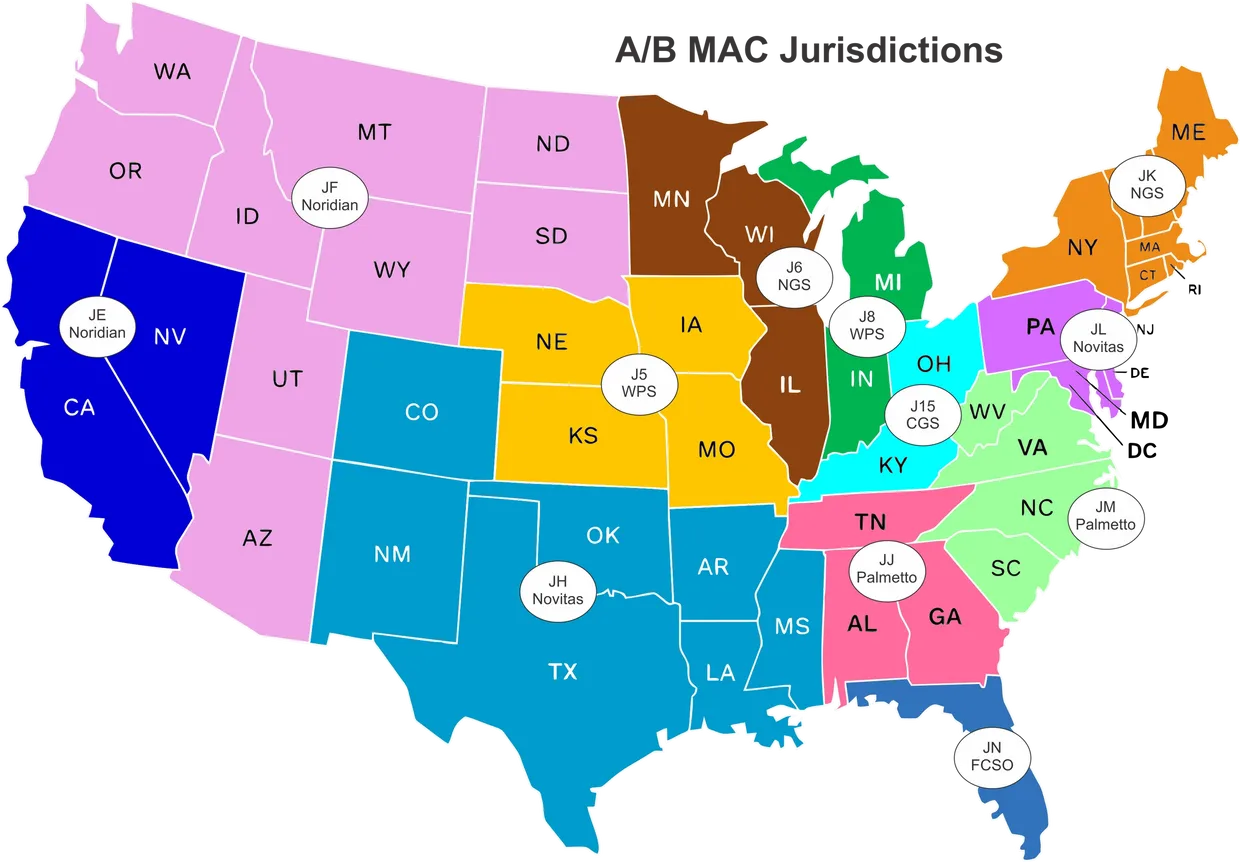
In the ever-changing world of Medicare-approved products, we have made a decision to carry multiple allografts for our Clinicians to have options to choose from. 1 Health Source only offers Medicare-approved allografts. Your representative will go through your options on a call. Once you’ve decided which allografts you want to move forward with, they will email the paperwork to you, and we will schedule your training calls.
Remember – there is no upfront cost to you or your practice.
Bill MD – Our 3rd-Party Billing Company
We understand the importance of submitting the claims accurately the first time. Our billing company specializes in wound care claims. It is not a requirement that you use Bill MD; however, we do recommend that you consider using Bill MD for either wound care-only claims or for all of your claims.
Customer Support
We are here to help you and your practice. Our offerings extend far beyond wound care solutions. Your Representative can go through some additional solutions to consider to help improve your patients’ care.

Wound Care – Matrix Derivatives

Human Placenta

Collagen
Porcine
Advanced Wound Care Therapy Descriptions
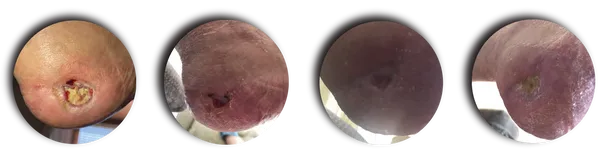
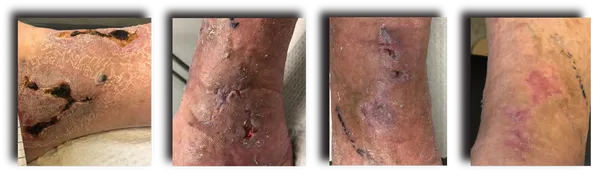
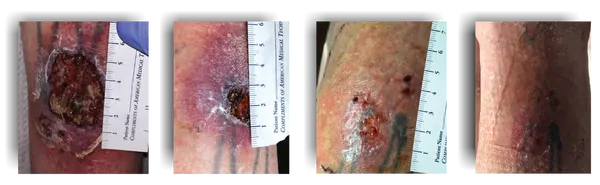
Debriding a Leg
Debriding Toes
Applying the Allograft
Advanced Wound Care Solutions

What is the future of advanced wound care?
Studies have projected that the advanced wound care market, aiming at surgical wounds and chronic ulcers, is likely to reach $22 billion by 2024 and is poised to reach $28.6 billion by 2028.
This expansion is expected to be driven by technological advancement, rising incidences of chronic wounds, growing government support, and a rising elderly population.
We offer a full line of products developed for advanced wound care. Contact us to schedule a call to meet our Team. We look forward to working with you and your locations.
What are the treatment options for chronic wounds?
At first, chronic wounds are regularly cleaned and covered using wound dressings and bandages. If a wound still hasn’t healed after a long time despite this wound care, special treatments such as vacuum-assisted closure or skin grafts are used.
If someone has a wound for more than eight weeks without any signs of it healing, it’s considered to be a chronic wound. These kinds of wounds usually arise as a result of poor blood circulation, diabetes or a weak immune system. Open wounds on the lower leg are also known as venous leg ulcers.
As well as treating the underlying condition and tending to the wound, pain relief is important. Some people with complex, poorly healing wounds find psychological support helpful too.
Cleaning the wound
The wound is often cleaned when the dressing is changed, normally using a saline (salt) solution. Overall, though, not enough is known about the advantages and disadvantages of the various solutions that are used to clean wounds, and how they affect the healing process. It’s also not yet clear whether tap water could be used for the medical cleaning of wounds.
Debridement
When treating chronic wounds, doctors or nurses often remove dead or inflamed tissue. This is known as debridement. The tissue is removed using instruments such as tweezers, a sharp spoon-like instrument called a curette, or a scalpel. An enzyme-based gel is sometimes applied too, to help clean the wound.
The wound can also be cleaned using a high-pressure water jet. Another form of debridement involves the use of a certain species of maggots (fly larvae) that are specially bred for medical purposes. The maggots are placed on the wound, either as they are or in a pouch. They remove dead tissue and fluid from the wound. Because debridement is often painful, a local anesthetic is used to numb the wound beforehand, for instance using an ointment. If more severe pain is expected, painkillers can also be taken before treatment. Larger wounds are sometimes cleaned under general anesthetic. There is not enough good research on the advantages and disadvantages of the various debridement techniques to be able to say how effective they are.

Wound dressings
Once the wound has been cleaned, it is covered with a dressing. Most wounds are kept moist, for instance with moist compresses. But the following kinds of dressings can be used instead:
- Films
- Gauze
- Hydrogel dressings
- Hydrocolloid dressings
- Dressings containing silver or alginates
- Foam dressings
The dressings are used to remove excess fluid from the wound and protect it from infection. They are usually left on the wound for several days. Dressings should be changed if it’s clear that they can’t soak up any more wound secretions, if they slip out of place, or if fluid leaks out of the bandage. It’s not yet possible to tell which types of wound dressings are most suitable for different kinds of wounds because there isn’t enough good research in this area.
There are also dressings that contain substances called growth factors. These hormone-like substances are meant to help the healing process by promoting the growth of the body’s cells. But there aren’t enough good studies to be able to say whether treatment with growth factors is more effective than conventional wound care for diabetic foot ulcers and other kinds of chronic wounds.
Honey has traditionally been used in wound care. But applying specially prepared honey before dressing the wound probably doesn’t have any advantages. The effect of using honey in the treatment of leg wounds has so far only been tested in people with venous leg ulcers, though.
Compression stockings and compression bandages
If poor blood circulation is what caused the chronic wound, then compression stockings or compression bandages can help it to heal faster. The pressure from the stockings and bandages helps the veins to carry blood back to the heart and improves circulation.
Antibiotics
Wounds are even less likely to heal well if they are infected with bacteria. Depending on how severe the infection is, antibiotics may be considered. They can either be applied to the wound using an ointment or placed on the wound using a compress. Initial study results show that wounds in people with diabetic foot syndrome heal faster as a result. It’s not yet clear whether this also applies to wounds caused by other underlying diseases.
It’s also not clear whether antibiotic tablets can help: Studies haven’t shown that they have any advantages in wound healing compared to other treatments.
Hyperbaric oxygen therapy
In hyperbaric oxygen therapy, the person with the wound goes into a special chamber to breathe in oxygen under high pressure. This is meant to increase the oxygen concentration in their blood and improve the blood supply to the wound area.
Research suggests that hyperbaric oxygen therapy can improve the healing of wounds in people with diabetic foot syndrome.
Ultrasound and electromagnetic therapy
Ultrasound therapy involves treating chronic wounds using sound waves. The sound waves make the tissue warmer. But ultrasound therapy hasn’t been proven to help the wound heal faster.
The same is true of electromagnetic therapy, where weak electromagnetic waves are applied to the wound using pillows or mats that have magnets in them.
Negative pressure wound therapy
It’s not possible to say whether negative pressure wound therapy can help in people with chronic wounds because there’s a lack of good studies in this area. It’s also not clear whether shock-wave, ozone or light therapy can help.
The pump continuously sucks fluid out of the wound, creating negative pressure across the surface of the wound. The aim is to increase the flow of blood to the wound. It helps keep the wound moist too, which is also meant to improve the healing process.
Pump systems are used in some hospitals to treat chronic or large open wounds, for example following skin grafts. But they can also be used at home. The negative pressure is either applied to the wound around the clock or at regular time intervals.
But the pump, which is constantly attached, limits your mobility and makes noise. Some people find this annoying. Changing the dressing and tube can also be painful and cause a small amount of bleeding.
It’s not possible to say whether negative pressure wound therapy can help in people with chronic wounds because there’s a lack of good studies in this area. It’s also not clear whether shockwave, ozone or light therapy can help.
Skin grafts
Skin grafts are considered as a treatment option if a wound is so large that it can’t close on its own. In this procedure, skin is taken from another part of your body – usually your thigh – and transplanted onto the wound.
There are also grafts that are made from human cell products and synthetic materials. Studies have shown that these increase the chances of poorly healing venous leg ulcers closing faster. The wounds healed completely within six months in:
- 40 out of 100 people who had conventional treatment using wound dressings,
and in
- 61 out of 100 people who had a skin graft.
Chronic foot wounds also healed faster after a skin graft than after standard treatment.
What are the pain management options?
Painful chronic wounds can be a burden in daily life and also prevent you from getting a good night’s sleep. Constant pain can really wear you down, making you feel quite low or even depressed after a while.
Drugs like acetaminophen (paracetamol) or ibuprofen can help ease mild to moderate pain. If they aren’t effective enough, the doctor can prescribe a stronger painkiller.
Wound dressings that contain ibuprofen are also available. There’s not enough research to be able to say how effectively they can relieve pain caused by chronic wounds.
People who have chronic pain can benefit from psychological support. Psychological treatments for pain management aim to help people cope better with the pain in everyday life.
Sources
Arbeitskreis “Krankenhaus- und Praxishygiene” der AWMF. Chronische und sekundär heilende Wunden: Hygieneanforderungen (S1-Leitlinie). AWMF-Registernr.: 029-042. January 31, 2014.
Aziz Z, Cullum N. Electromagnetic therapy for treating venous leg ulcers. Cochrane Database Syst Rev 2015; (7): CD002933. [PMC free article] [PubMed]
Briggs M, Nelson EA, Martyn-St James M. Topical agents or dressings for pain in venous leg ulcers. Cochrane Database Syst Rev 2012; (11): CD001177. [PMC free article] [PubMed]
Cullum N, Liu Z. Therapeutic ultrasound for venous leg ulcers. Cochrane Database Syst Rev 2017; (5): CD001180. [PMC free article] [PubMed]
Deutsche Gesellschaft für Wundheilung und Wundbehandlung (DGfW).
Lokaltherapie chronischer Wunden bei Patienten mit den Risiken periphery arterielle Verschlusskrankheit, Diabetes mellitus, chronische venöse Insuffizienz (S3-Leitlinie). AWMF-Registernr.: 091-001. June 12, 2012.
Dumville JC, Deshpande S, O’Meara S, Speak K. Foam dressings for healing diabetic foot ulcers. Cochrane Database Syst Rev 2013; (6): CD009111. [PMC
free article] [PubMed]
Dumville JC, Hinchliffe RJ, Cullum N, Game F, Stubbs N, Sweeting M et al. Negative pressure wound therapy for treating foot wounds in people with diabetes mellitus. Cochrane Database Syst Rev 2013; 10: CD010318. [PubMed]
Dumville JC, Land L, Evans D, Peinemann F. Negative pressure wound therapy for treating leg ulcers. Cochrane Database Syst Rev 2015; (7): CD011354. [PMC free article] [PubMed]
Dumville JC, Lipsky BA, Hoey C, Cruciani M, Fiscon M, Xia J. Topical antimicrobial agents for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev 2017; (6): CD011038. [PMC free article] [PubMed]
Dumville JC, O’Meara S, Deshpande S, Speak K. Hydrogel dressings for healing diabetic foot ulcers. Cochrane Database Syst Rev 2013; (7): CD009101. [PMC free article] [PubMed]
Gethin G, Cowman S, Kolbach DN. Debridement for venous leg ulcers. Cochrane Database Syst Rev 2015; (9): CD008599. [PMC free article] [PubMed]
Institute for Quality and Efficiency in Health Care (IQWiG, Germany). Hyperbare Sauerstofftherapie bei diabetischem Fußsyndrom: Final report; Commission N15-02. March 20, 2016. (IQWiG reports; Volume 382).
Jones JE, Nelson EA, Al-Hity A. Skin grafting for venous leg ulcers. Cochrane Database Syst Rev 2013; (1): CD001737. [PMC free article] [PubMed]
Jull AB, Cullum N, Dumville JC, Westby MJ, Deshpande S, Walker N. Honey as a topical treatment for wounds. Cochrane Database Syst Rev 2015; (3): CD005083. [PMC free article] [PubMed]
Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE, Weibel S. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database Syst Rev 2015; (6): CD004123. [PMC free article] [PubMed]
Liu J, Zhang P, Tian J, Li L, Li J, Tian JH et al. Ozone therapy for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev 2015; (10): CD008474. [PMC free article] [PubMed]
Martinez-Zapata MJ, Marti-Carvajal AJ, Sola I, Exposito JA, Bolibar I, Rodriguez L et al. Autologous platelet-rich plasma for treating chronic wounds. Cochrane Database Syst Rev 2016; (5): CD006899. [PMC free article] [PubMed]
Nelson EA, Hillman A, Thomas K. Intermittent pneumatic compression for treating venous leg ulcers. Cochrane Database Syst Rev 2014; (5): CD001899. [PubMed]
O’Meara S, Al-Kurdi D, Ologun Y, Ovington LG, Martyn-St James M, Richardson R. Antibiotics and antiseptics for venous leg ulcers. Cochrane Database Syst Rev 2014; (1): CD003557. [PubMed]
O’Meara S, Cullum N, Nelson EA, Dumville JC. Compression for venous leg ulcers. Cochrane Database Syst Rev 2012; (11): CD000265. [PMC free article] [PubMed]
O’Meara S, Martyn-St James M. Foam dressings for venous leg ulcers. Cochrane Database Syst Rev 2013; (5): CD009907. [PubMed]
O’Meara S, Martyn-St James M, Adderley UJ. Alginate dressings for venous leg ulcers. Cochrane Database Syst Rev 2015; (8): CD010182. [PMC free article] [PubMed]
Rhee SM, Valle MF, Wilson LM, Lazarus G, Zenilman JM, Robinson KA. Negative Pressure Wound Therapy Technologies for Chronic Wound Care in the Home Setting. September 15, 2014. (AHRQ Technology Assessment Reports).
Santema TB, Poyck PP, Ubbink DT. Skin grafting and tissue replacement for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev 2016; (2): CD011255. [PMC free article] [PubMed]
Wang HT, Yuan JQ, Zhang B, Dong ML, Mao C, Hu D. Phototherapy for treating foot ulcers in people with diabetes. Cochrane Database Syst Rev 2017; (6): CD011979. [PMC free article] [PubMed]
Wu B, Lu J, Yang M, Xu T. Sulodexide for treating venous leg ulcers. Cochrane Database Syst Rev 2016; (6): CD010694. [PMC free article] [PubMed]
Zenilman J, Valle MF, Malas MB, Maruthur N, Qazi U, Suh Y et al. Chronic venous ulcers: a comparative effectiveness review of treatment modalities December 2013. (AHRQ Comparative Effectiveness Reviews; Volume 127). [PubMed]
Zhang J, Hu ZC, Chen D, Guo D, Zhu JY, Tang B. Effectiveness and safety of negative-pressure wound therapy for diabetic foot ulcers: a meta-analysis. Plast Reconstr Surg 2014; 134(1): 141-151. [PubMed]
Zhao XH, Gu HF, Xu ZR, Zhang Q, Lv XY, Zheng XJ et al. Efficacy of topical recombinant human platelet-derived growth factor for treatment of diabetic lower-extremity ulcers: Systematic review and meta-analysis. Metabolism 2014; 63(10): 1304-1313. [PubMed]
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services. Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. We do not offer individual consultations. Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods. © IQWiG (Institute for Quality and Efficiency in Health Care) Bookshelf ID: NBK326436
BerbereX for Wound Care

CLINICALLY PROVEN to Support HEALING of CUTS, BURNS, INCISIONS, SCRAPES and WOUNDS, including Skin Sores, Pressure Sore, Bed Sore and Diabetic Ulcers. This is a great solution for radiation burns.
- SAFE and Non-irritating ANTIMICROBIAL WOUND CLEANSER to help prevent infection and be used as FIRST AID ANTISEPTIC SPRAY for wound care and be part of every FIRST AID BAG and FIRST AID KIT
- DR. RECOMMENDED and FDA Registered formula backed by clinical research that proves BerbereX to be effective in killing bacteria and putting you on the road to recovery sooner.
- Allows FAST, thorough and GENTLE cleansing of acute and chronic wounds of all stages.
- KILLS bacteria and PROTECTS skin for faster healing, REDUCES the risk of infection, promoting faster healing, CALMS redness, inflammation, and discomfort, REDUCES the risk of scarring.
Ideal Markets:
- Wound Care Clinics
- Pharmacies
- Retail Chain Drug Stores
- Nursing Homes